“Once it came to New York, I knew I would get it,” said Dr. Dara Kass, an Emergency Medicine Physician in Manhattan’s New York-Presbyterian Hospital, and Associate Professor of Emergency Medicine at Columbia University Irving Medical Center. The Park Slope resident and mother of three, is working on the frontlines of the novel coronavirus pandemic in New York City. The highly contagious respiratory illness, coronavirus disease 2019 (COVID-19), was first identified during an investigation into a coronavirus outbreak in Wuhan, China, with the first case dating back to November 2019.
“This is running like wildfire through our city and we’re seeing younger generations test positive for infection,” Kass said. “The level of impact is unlike anything we’ve ever seen.”
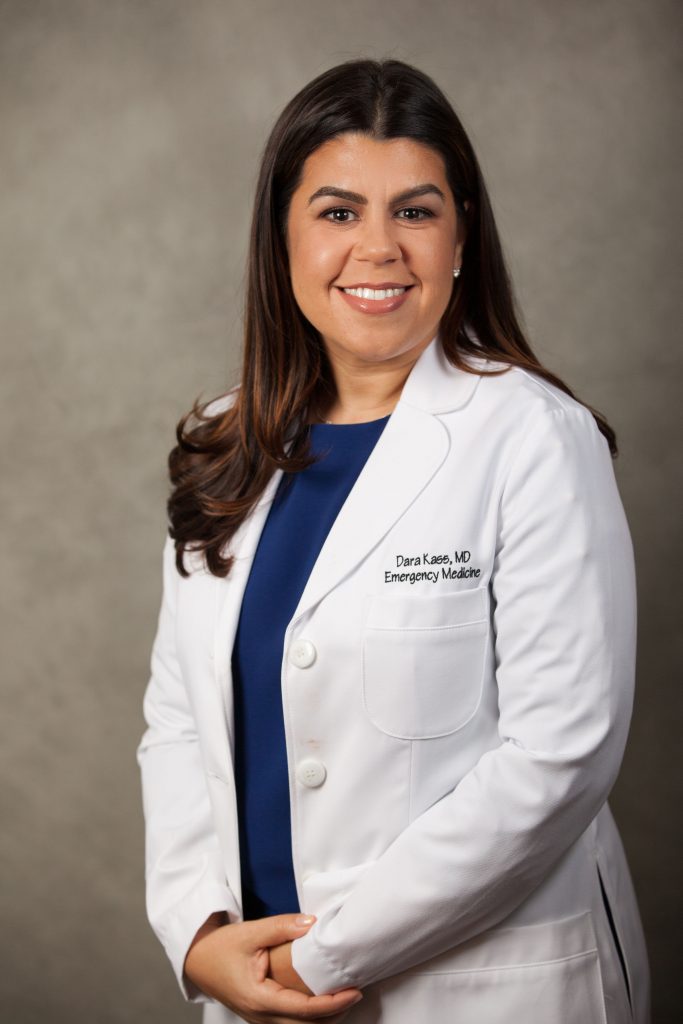
Kass tested positive for COVID-19, after caring for patients in the ER. A few weeks later, news broke that the New York metropolitan area, surging in novel coronavirus cases, had emerged to the epicenter of the global pandemic. By March 31, New York City had topped over 38, 000 confirmed cases of the infection. The Trump Administration’s lack of preparedness, including budget cuts for the Centers for Disease Control and Prevention (CDC) and allowing for a contract to lapse, maintaining stockpiles of ventilators, has fundamentally contributed to the spread of the COVID-19 pandemic. Hospitals throughout NYC are overrun with an influx of infected patients and strained by the limited resources available. Shortages in test kits, personal protective equipment, and life-saving ventilator machines are making both patients and medical personnel vulnerable to infection. In many ways, the Federal Government, lacking a uniform response to the novel coronavirus, set up the healthcare system for failure.
As a native New Yorker, Dr. Kass has lived and worked through some of the city’s greatest catastrophes, including the coordinated terrorist attacks of September 11 and the unprecedented flooding of Hurricane Sandy.
“This is a continuous thing,” Kass said. “These other events, like 9/11, were traumatic, but this is much bigger and riskier to people’s lives. It’s very dangerous and unpredictable. It will keep infecting people.”
Dr. Kass watched as the coronavirus spread throughout China, Asia, and Europe, planning for when the virus would eventually come to NYC.
“We had to mobilize quickly,” Kass explained. “We were all thinking about policy, and we didn’t know exactly how it would come to NYC, but we knew that it would come and that we would see it through. I sent my kids to stay with family.”
After testing positive for COVID-19, Dr. Kass took drastic measures to protect her husband. She wore a mask indoors while quarantining herself in a separate living area of their home. She was able to continue assisting her patients remotely through telemedicine, a medical practice that relies on technology to connect patients and physicians without in-person visits.
The state mandate to close all non-essential businesses and NYPD enforced social distancing guidelines, are part of Governor Andrew Cuomo’s stay-at-home executive order, termed “New York State on PAUSE.” New data offers evidence that vigilant measures, including restrictions to social- distancing and non-essential gatherings, are slowing the spread of the virus.
“Flattening the curve keeps our hospitals open,” Kass explained. “What we know is that a vaccine will take about a year to develop, but until then, we have to stop people from getting infected.” She added, “Cuomo has been extraordinary. He is exactly what we need. He has treated the New York hospital systems as a whole, and I look forward to his press conferences every day. He has really been remarkable.”
In a New York Times feature, Dr. Kass and her co-authors urge government officials and authorities to make mask-wearing a national policy. The editorial explains that in a randomized control trial, participants who wore a surgical mask were 80% less likely to contract a respiratory illness. Kass and co-authors ask the public to restrict buying N-95 masks while offering resourceful alternatives, including cloth masks and handmade face coverings. While surgical masks should be given to workers in essential jobs, cloth masks can reduce the viral spread of the virus and avoid a second wave of infections.
Recently, President Trump announced in a news briefing that new guidance from the CDC urges Americans to wear cloth face coverings in public. President Trump rejected the advice from the CDC and his administration’s counsel, by adding, “This is voluntary. I don’t think I’m going to be doing it.”
At the time of publication, New York State has 123,160 laboratory- tested and confirmed cases of COVID-19, including 4,159 deaths. There are 67,551 cases in the five boroughs.
16, 479 New Yorkers are currently being hospitalized throughout the state.
Although Dr. Kass has made a full recovery from COVID-19, she is planning to move out of her home for the duration of the pandemic. The decision was made in part to protect her family, and also to be readily available for her patients and colleagues.

I decided to ask Dr. Kass something that I’ve wondered about regarding all medical professionals and essential workers: has the coronavirus pandemic made her regret going into the medical field.
“No, not even a little bit,” she told me. “I did my job, and I’m going to go back to do this job until the end. Emergency medical people live for this. This will always be who we are.”
Dr. Dara Kass (@darakass) is an ER Doctor, Professor of Emergency Medicine, public speaker, political activist, and founder of FemInEM, an online platform that cultivates a community for females working in emergency medicine.
For information on cloth masks in Park Slope: Diana Kane https://www.dianakane.com/products/liberty-print-mask